

This is a long and short axis view of an acute isolated gracilis tendon rupture. The above image is the long axis view in a coronal plane that demonstrates a gracilis tendon stump that is retracted into the distal medial thigh. Loss of tension is seen in the tendon suggestive of rupture and retraction. There is adjacent anechoic and hypoechoic fluid consistent with hemorrhage. The below image is the short axis view in a transverse plane that demonstrates anechoic to hypoechoic fluid within the gracilis interval consistent with hemorrhage from gracilis tendon rupture.

This is a coronal plane view of the temporomandibular joint (TMJ) during a TMJ injection. The needle can be seen in a caudad lateral to cephalad medial in-plane orientation with the needle tip deep to the TMJ capsule. The injection solution contained a mixture of dextrose solution instead of corticosteroid, due to the potential risks of corticosteroid complications in this area. It is not uncommon to see some iatrogenic temporary facial nerve paralysis following this injection if any anesthetic leaks out of the joint.

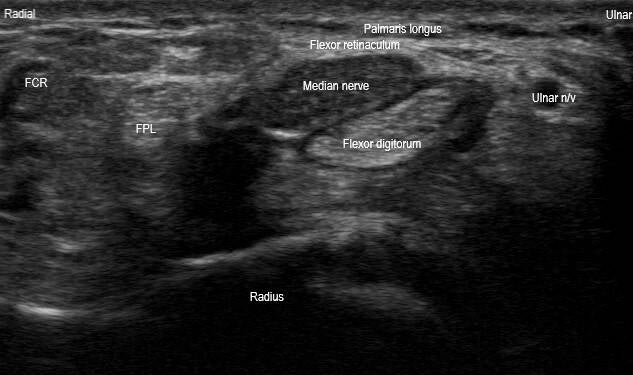
These are long and short axis images of the carpal tunnel. The long axis image (top) demonstrates fusiform swelling, hypoechoic thickening, loss of normal fascicular pattern, and notching of the median nerve at the carpal tunnel inlet. The short axis image (bottom) demonstrates hypoechoic thickening and loss of normal fascicular pattern of the median nerve. There is also bowing of the wrist flexor retinaculum. The median nerve cross-sectional area measures approximately 33 millimeters², which is significantly larger than the normal average of 8-9 millimeters². These findings suggest severe carpal tunnel syndrome.

This is a long axis image in a sagittal plane of the distal Achilles tendon at the insertion. This image was taken immediately following an injection of the retrocalcaneal bursa. A longitudinal split tear is seen within the insertional fibers of the Achilles tendon, which was better visualized following the injection. Additionally, there is increased hypoechogenicity within the anterior insertional Achilles tendon fibers, suggestive of insertional Achilles tendinosis.

This is a transverse image just cephalad to the sternum to appreciate the sternoclavicular (SC) joints side by side. This image demonstrates a posterior orientation of the right medial clavicle and SC joint relative to the sternum and contralateral SC joint. Edema and hemorrhage of the of the right medial clavicle and SC joint can be visualized. This image is consistent with an SC joint posterior dislocation. Due to the proximity of large vasculature and airway posteriorly, this injury requires urgent imaging with CT chest and/or CT angiography for confirmation of dislocation and evaluation of mediastinal vascular injury, considering the patient is stable.

This is a transverse plane image of a bicipitoradial bursa injection at the dorsal elbow with the elbow flexed and hyperpronated. The needle can be seen in a dorsal ulnar to volar radial in-plane orientation with the needle tip within the bicipitoradial bursa. This technique is safer because it avoids the posterior interosseous nerve (PIN) dorsoradially and neurovasculature volarly.

This is a transverse plane image of the gluteal region at the ischial spine following a pudental nerve block at the interligamentous interval of the sacrotuberous ligament (STL) and sacrospinous ligament (SSL). The pudental nerve (PN) can become entrapped here, resulting in pudental neuralgia. Anechoic fluid from the injectate can be seen within the interligamentous interval in this image. Care should be taken to avoid penetrating the internal pudental artery (IPA).

This is a short axis image in a transverse plane at the distal radial forearm where the first dorsal compartment courses superficial to the second dorsal compartment. A small amount of anechoic fluid can be seen within the first dorsal compartment tendon sheath. This particular patient had pain, squeaking, and crepitus with thumb and wrist extension due to the friction of the tendons at this intersection. This is known as proximal intersection syndrome. Fluid can be seen in either compartment in this diagnosis. If an injection is attempted, the superficial radial nerve should be identified and avoided.

This is a long axis image of the plantar fascia central cord at the origin on the medial calcaneal tubercle. This image demonstrates an irregular thickened echogenic area with surrounding hypoechogenicity throughout the full thickness of the central band of the plantar fascia. There appears to be some loss of tension of the plantar fascia. There is absent color Doppler flow. These findings are most suggestive of postsurgical scar tissue. This particular patient underwent plantar fascia release surgery 3-4 years prior and has recently experienced a recurrence of pain at this site. The other differential to consider is a plantar fibroma; however, plantar fibromas are more commonly seen at the middle and distal plantar fascia and appear more discrete. They are also typically seen more superficial and not throughout the full thickness of the plantar fascia.


This is a long axis image in a sagittal plane using the medial window and a short axis image in a transverse plane of the distal biceps tendon. These orthogonal images demonstrate a partial thickness anechoic defect and increased hypoechogenicity within the distal biceps tendon with a small amount of anechoic fluid within the adjacent bicipitoradial bursa. These findings are consistent with a partial thickness distal biceps tendon tear.

This is an oblique transverse plane view of the high ankle long axis to the anterior inferior tibiofibular ligament (AITFL). This image demonstrates an anechoic defect within the deep band of the AITFL extending partially through the superficial band. This is consistent with a partial tear of the AITFL seen in a high ankle sprain. Stress testing can be performed under ultrasound to evaluate widening of the tibiofibular space and competency of the ligament and syndesmosis.

This is a transverse plane image short axis to the dorsal compartments of the wrist during a distal radial ulnar joint (DRUJ) injection. The needle can be seen in a dorsal ulnar to volar radial in-plane orientation with the needle tip in the DRUJ. A gel standoff can aid in visualizing the needle by making the ultrasound waves more perpendicular to the needle.

This is a transverse plane image short axis to the proximal hamstring origin at the ischial tuberosity during an ischial bursa injection. The needle can be seen in a posterolateral to anteromedial in-plane orientation with the needle tip in the ischial bursa (plane between the hamstring and gluteus maximus). The injectate should flow peritendinously.

This is an oblique sagittal plane view long axis to the proximal patellar tendon. This image depicts a swollen hypoechoic infrapatellar branch of the saphenous nerve. This patient had findings consistent with infrapatellar branch saphenous neuritis due to repetitive kneeling. Symptoms included a sharp tingling numbness-like pain that radiated from medial to lateral across the anterior knee with compression of this area.

This is a transverse plane view of the proximal medial forearm during a median nerve hydrodissection. The needle can be seen in a medial volar to lateral dorsal in-plane approach with the needle tip just outside the median nerve epineurium hydrodissecting the nerve from the proximal edge of the pronator teres and from the brachialis. Care should be used to avoid puncturing the adjacent vasculature. This particular patient had a proximal median nerve entrapment with acute denervation of the pronator teres muscle.
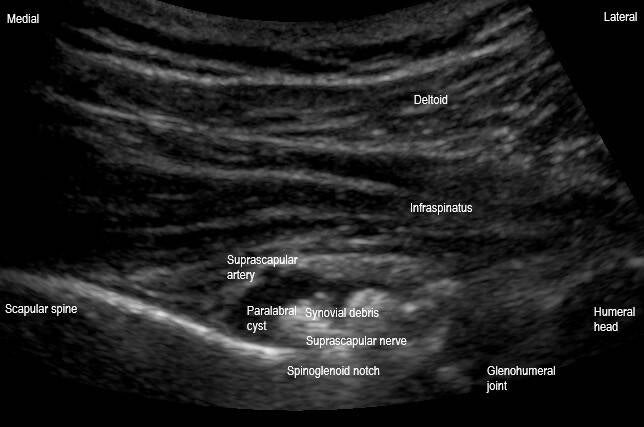
This is a transversal plane view of the spinoglenoid notch of the scapula. This image demonstrates a cystic lesion within the spinoglenoid notch containing hypoechoic and echogenic material compressing the suprascapular nerve deep in the notch. This is most consistent with a complex paralabral cyst of the spinoglenoid notch. This can be a cause of suprascapular nerve entrapment and neuritis, as was the case in this patient.

This is a transversal plane view of the posterior glenohumeral joint. This image demonstrates posterior glenoid cortical irregularity, increased hypoechogenicity and loss of normal triangular shape of the posterior glenoid labrum. This suggests a degenerative glenoid labral tear.

This is a transverse oblique view of the posteromedial elbow at the cubital tunnel with the elbow flexed to 45°. This image demonstrates hypoechoic swelling of the ulnar nerve with loss of fascicular echotexture. The cross-sectional area of the nerve measures 15mm² at the medial epicondyle, which is larger than the average of approximately 6-9mm² mentioned in various studies. This suggests ulnar neuritis at the elbow or cubital tunnel syndrome. Dynamic evaluation of the ulnar nerve should always be performed using elbow flexion and extension to evaluate for ulnar nerve instability.

This is a transversal plane view of the popliteal fossa short axis to the popliteal artery just proximal to the popliteal artery bifurcation. A large pulsatile cystic mass measuring 4.0 x 4.8 x 5.9 cm is seen. There is heavy mixing of color Doppler within the mass lumen. There is echogenic material on the lumen walls. This is consistent with a partially thrombosed saccular popliteal artery aneurysm.

This is a coronal oblique plane image short axis to the peroneal tendons (peroneal longus (PL) and peroneal brevis (PB)) long axis to the calcaneofibular ligament (CFL). Anechoic fluid can be visualized within the peroneal tendon sheath, consistent with peroneal tenosynovitis. Additionally, there is a subtle linear anechoic defect within the PB, consistent with a longitudinal split tear of the PB. The CFL is partly anisotropic.

This is an anatomic coronal oblique plane image of the acromioclavicular (AC) joint demonstrating a large anechoic mass with scattered hyperechoic debris within. This is known as the Geyser Sign and suggests a massive rotator cuff tear, usually seen in the setting of rotator cuff arthropathy. The anechoic (fluid) portion of this cyst was compressible and there is posterior acoustic enhancement seen deep to this.

This is an oblique transversal plane view short axis to the hamstring tendon origin on the ischial tuberosity. This image demonstrates hypoechoic thickening of the semimembranosus and conjoint tendon of the biceps femoris long head and semitendinosus, and cortical irregularity of the ischial tuberosity. There is anisotropy artifact within the semimembranosus due to the ultrasound beam not being perpendicular to the fibers, which is commonly seen here. Other views demonstrated increased color Doppler flow within these tendons suggesting tendinopathic hyperemia. These findings indicate proximal hamstring tendinopathy with likely associated ischial bursitis.

This is a transverse plane view of the anterior ankle at the level of the anterior talar cartilage of the tibiotalar joint. This image demonstrates a hyperechoic line parallel to the articular cartilage at the chondrosynovial interface (white arrow). This is known as the double contour sign, a hallmark finding seen in gout. This linear hyperechoic enhancement represents monosodium urate crystal deposition overlying the hyaline cartilage, creating a distinct, double-layered appearance.
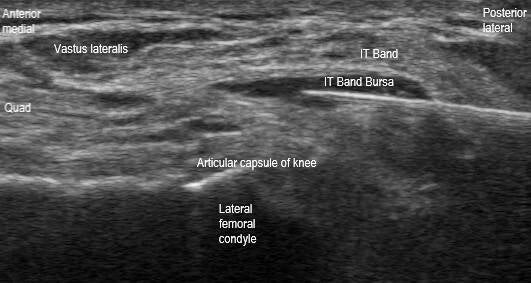
This is a transverse plane image short axis to the distal iliotibial (IT) band at the distal femur during an IT band bursa injection in a patient with a total knee arthroplasty (TKA). The needle can be seen in a posterolateral to anteromedial in-plane orientation with the needle tip within the IT band bursa. IT band friction syndrome is a common cause of overuse lateral knee pain following a TKA. During this procedure, care should be taken to avoid injecting deep to the articular capsule (intraarticular).

This is a coronal oblique plane image long axis to the proximal medial collateral ligament (MCL). The origin of the MCL at the medial femoral epicondyle demonstrates hypoechoic thickening of 8 millimeters (mm) and loss of normal fibrillar echotexture. This is suggestive of an MCL sprain, likely grade 1-2. MCL injury is suggested when there is thickening greater than 6 mm at the femoral side. Dynamic valgus stress test under ultrasound can be performed to assess joint space widening to assign a grade to the MCL sprain.

This is a long axis view in an anatomic oblique coronal plane of the supraspinatus tendon. An anechoic defect can be seen at the articular side that extends greater than 50% of the thickness of the tendon. This is consistent with a high grade partial articular sided supraspinatus tear. An orthogonal view in the short axis should be evaluated to assess the width of the tear. Additionally, a thin hyperechoic line is seen at the interface between the normal hypoechoic hyaline articular cartilage of the humeral head and abnormal anechoic tear of the supraspinatus tear. This is known as the cartilage interface sign and is due to the difference between the acoustic impedances of the two tissues at the interface. This sign indicates a partial or complete supraspinatus tear and has a very high specificity but low sensitivity.

This is a coronal oblique plane image of the distal peroneal longus (PL) and peroneal brevis (PB) at the level of the peroneal tubercle. At this level, the peroneal tendons typically have their own sheath. The PL tendon sheath is thickened and hypoechoic consistent with tenosynovitis. The peroneal tubercle is prominent and measures approximately 5 mm from tip to base, which is suspicious of a hypertrophied peroneal tubercle. A hypertrophied peroneal tubercle may result in tenosynovitis of the PL at this level.

This is a transverse plane image short axis to the first dorsal compartment tendons (abductor pollicis longus (APL) and extensor pollicis brevis (EPB)) of the wrist during a first dorsal compartment injection. The needle can be visualized in a dorsal to volar in-plane orientation with the needle tip seen within the EPB tendon sheath. A septate first dorsal compartment is seen with tenosynovitis of the EPB tendon. This is common anatomical variant. Recognition of this is key so the affected tendon sheath can be targeted.

This is a oblique coronal view long axis to the distal radius depicting a distal radius fracture in a 15-year-old. A hyperechoic osseous periosteum interruption can be visualized at the distal radial metaphysis with adjacent echogenic material, consistent with a distal radius fracture with an associated volar fracture hematoma. Plain radiographs revealed an apex dorsal angulation of approximately 30 degrees. An ultrasound guided volar hematoma block was performed followed by a successful closed reduction.

This is an anatomic oblique transverse plane view short axis to the long head biceps tendon (LHBT) at the rotator interval. The coracohumeral ligament (CHL) is mildly thickened. Additionally, the superior glenohumeral ligament (SGHL) appears hypoechoic and mildly thickened. These findings can be seen in adhesive capsulitis of the glenohumeral joint. Some studies report that CHL thickening of >2.2 millimeters suggests adhesive capsulitis.

This is a sagittal plane view of the dorsal wrist during a radiocarpal joint injection. The needle can be visualized in a distal dorsal to proximal volar in-plane orientation. The needle tip is seen within the dorsal radiocarpal joint recess. Anechoic fluid can be viewed distending from both the dorsal radiocarpal and midcarpal joints, consistent with effusions. Cortical irregularity is seen at the radiocarpal joint and midcarpal joint margins. This particular patient had wrist osteoarthritis secondary to scapholunate advanced collapse.

This is a transverse plane image short axis to the proximal part of the Achilles tendon during a sural nerve hydrodissection. The needle can be seen in an anterolateral to posteromedial in-plane orientation with the needle tip just lateral to the sural nerve with fluid surrounding the sural nerve within the fibrous arcade of the sural aponeurosis. This can be a site of sural nerve entrapment such as following Achilles tendon injury, surgical repair, or boot immobilization. Care should be taken to avoid injecting the small saphenous vein. Light transducer pressure can help reduce compression of the vein.

This is a anatomic coronal plane view long axis to the posterior tibialis tendon at it's proximal insertion on the navicular tuberosity. This image demonstrates a posterior tibialis tendon tenosynovial effusion with echogenic debris as well as increased hypoechogenicity and loss of fibrillar echotexture at the tendon insertion. These sonographic findings are most consistent with posterior tibialis tenosynovitis and insertional tendinopathy. Dynamic imaging as well as a short axis view throughout the tendon's course should be performed to confirm these long axis findings and to evaluate for any longitudinal tears.
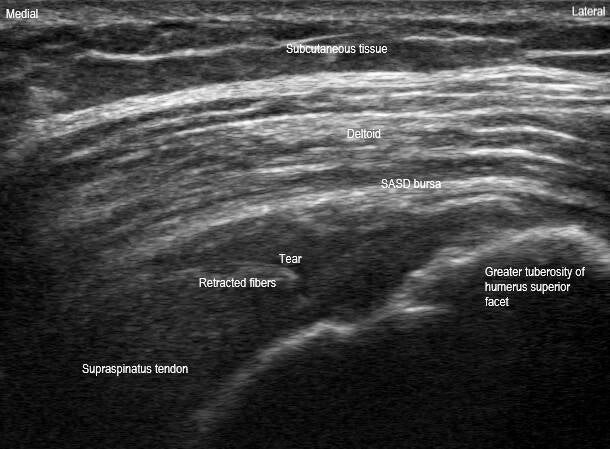

This is a long axis view in a anatomic oblique coronal plane and a short axis view in a anatomic oblique sagittal plane of the superior rotator cuff. These orthogonal views demonstrate an acute full thickness full width supraspinatus tendon tear. Retracted tendon stump fibers can be seen in the long axis view with a full thickness anechoic and hypoechoic defect and loss of fiber continuity. Dynamic maneuvers would show that the tendon does not move continuously together in long axis. The width and thickness of the tear can be appreciated on the short axis view. This is most likely acute given the findings of preserved superior convexity of the supraspinatus without dipping of the subacromial subdeltoid (SASD) bursa or synovial hypertrophy or infiltration. Additionally, acute tears may not show as much tendon retraction and should not have fatty infiltration or atrophy of the muscle belly. This particular patient fell on her shoulder approximately 2-3 weeks prior to this ultrasound scan.

This is a transverse plane image of a Baker's cyst during a Baker's cyst aspiration. The needle can be seen in a posteromedial to anterolateral in-plane orientation with the needle tip within the medial portion of the cyst. This particular cyst appears as a crescent or bilobed concave shape. A Baker's cyst, also known as a popliteal cyst, is a fluid-filled swelling that develops behind the knee, often associated with joint disorders like arthritis. It appears as a well-defined, anechoic or hypoechoic area within the popliteal fossa, located between the medial head of the gastrocnemius muscle and the semimembranosus tendon. In the transverse plane, the cyst is typically oval, crescent, bilobed concave, or beak shaped and maintains a well-defined, smooth contour. Its shape can vary depending on the amount of fluid, thickness of fluid, and the degree of distension. Aspirations are typically performed medial to lateral in-plane to avoid the neurovasculature located more lateral within the popliteal fossa.

This is a transverse plane view short axis to the radial nerve at the lateral supracondylar ridge of the humerus just distal to the radial groove of the humerus. The radial nerve appears to have hypoechoic swelling with some loss of fascicular pattern. The radial nerve wraps around the humerus at the radial groove to course anteriorly between the brachioradialis and brachialis anteriorly. This particular patient had a wrist drop and demonstrated signs of fatty infiltration of the extensor muscles of the forearm.

This is a transverse plane view short axis to the radial nerve at the lateral supracondylar ridge of the humerus during a perineural injection and hydrodissection of the radial nerve. The needle tip can be seen just deep to the radial nerve epineurium in a posterior to anterior in-plane orientation. Bayonet artifact (the appearance of bending) and reverberation artifact (multiple hyperechoic lines deep) can be seen from the needle. Care should be taken to avoid puncturing the nearby vasculature.

This is a transverse plane short axis view of the long head biceps tendon (LHBT) at the bicipital groove and lesser tuberosity of the proximal humerus. The LHBT is seen dislocated out of the bicipital groove medially within the superficial fibers of the subscapularis tendon. LHBT instability is most commonly seen due to insufficiency of the biceps soft tissue pulley system consisting of the subscapularis tendon and superior glenohumeral and coracohumeral ligaments. The most common reason for medial instability is due to a degenerative tear of the subscapularis tendon. Dynamic testing with external and internal rotation may demonstrate LHBT medial dislocation and reduction, respectively, or it may be chronically dislocated. Another contributing factor can be the shape of the bicipital groove. A relatively shallow bicipital groove is shown in this image.

This is a anatomic coronal plane image of an acromioclavicular (AC) joint during an AC joint injection. The AC joint capsule can be seen distended cephalad due to synovial hypertrophy within the AC joint. The needle tip can be visualized in a short axis out-of-plane orientation, represented by a subtle hyperechoic dot within the joint space. A walk-down technique can be used in this out-of-plane technique until the needle tip is visualized within the joint. Additionally, using the centerline function on the ultrasound will display a vertical line in the middle of the screen which helps localize the needle as this line corresponds with the line indicated at the center of the transducer. Resistance to flow could indicate the needle is within the articular disc and should be avoided.

This is an anatomic sagittal oblique plane image of a hip joint effusion long axis to the femoral neck. Anechioc fluid is seen distending the hip joint capsule. A hyperechoic synovial loose body can be seen deep to the capsule. The distance between the anterior surface of the femoral neck and the posterior margin of the iliopsoas tendon can be measured to evaluate for hip effusion. If the space measures greater than 5 millimeter (mm) or greater than 2 mm compared to the contralateral hip, it is considered a hip effusion. The space is measured at 15 mm in this particular image, which is diagnostic of a hip effusion.

This is a transverse plane image over the plantar aspect of the 5th metatarsal head during a 5th submetatarsal bursa injection. The needle tip is visualized within the submetatarsal bursa in a lateral to medial in-plane orientation. An anechoic fluid layer is seen within the bursa, which lies between the superficial transverse metatarsal ligament and the plantar subcutaneous fat pad tissue.

This is a transverse plane image of the sacroiliac (SI) joint during an SI joint injection. The needle can be seen in a posteromedial to anterolateral in-plane orientation with the needle tip visualized deep to the posterior SI ligament within the synovial inferior third of the SI joint. A helpful tip for identifying the synovial part of the SI joint articulation is by first positioning the transducer in a transverse plane over the posterior superior inferior iliac spine (PSIS) and sweeping the transducer in a caudad direction until the hyperechoic bony cortex of the PSIS drops off and a hypoechoic dip is visualized between the ilium and sacrum, which is the inferior part of the SI joint.

This is an anatomic coronal plane view, long axis to the supraspinous fossa of the scapula, during a suprascapular nerve (SSN) block at the suprascapular notch. The needle can be seen in a cephalad medial to caudad lateral in-plane orientation with the needle tip visualized deep to the transverse scapular ligament. The ligament is distended cephalad due to the injected fluid. This is the most common technique for a SSN block at the suprascapular notch, which is before the SSN innervates the supraspinatus and infraspinatus. The SSN provides approximately 70% of the sensory innervation to the glenohumeral joint and provides motor innervation to the supraspinatus and infraspinatus. This block is typically performed for pain relief, procedural analgesia, or postsurgical pain control. Serious complications can include pneumothorax or nerve injury, so it is very important to maintain visualization of the needle tip at all times during the procedure.

This is a long axis view of the quadratus femoris muscle within the ischiofemoral space in an anatomic transverse plane with the hip internally rotated during an ischiofemoral space injection. Ischiofemoral space syndrome is a rare condition caused by impingement of the structures within the space, commonly the quadratus femoris muscle, resulting in posterior hip pain. The needle can be seen in a posterior lateral to anterior medial in-plane orientation with the needle tip within the quadratus femoris muscle belly. Care should be taken to avoid puncturing the sciatic nerve, seen posterior medially. Internal rotation of the hip can help open the ischiofemoral space and stretch the quadratus femoris to allow more space for performing the injection.

This is a sagittal plane view of the palmar radial wrist during a scaphotrapeziotrapezoidal (STT) joint injection. The needle can be seen in a distal palmar to proximal dorsal in-plane orientation with the needle tip within the STT joint articulation. This injection can be useful diagnostically if there is also concomitant first carpometacarpal joint pathology. This can be performed in-plane as shown or out-of-plane in a palmar radial to dorsal ulnar approach. Care should be taken to avoid puncturing the superficial palmar branch of the radial artery that courses over the scaphoid tubercle.

This is an anatomic long axis view of the femoral head neck junction of a total hip arthroplasty during a periprosthetic hip aspiration. The prosthesis can be seen with reverberation and posterior acoustic shadowing artifacts deep to the components. The needle can be seen in an anterior caudad to posterior cephalad in-plane orientation. Targeting the most cephalad portion of the junction of the femoral head and stem components usually provides the highest fluid yield for aspiration if a large effusion is not visible deep to the capsule.

This is an oblique coronal plane view of the proximal tibia demonstrating an oblique view of the pes anserine tendons and long axis view of the distal medial collateral ligament (MCL) during an injection of the pes anserine bursa. The needle can be seen traversing posterior caudad to anterior cephalad in-plane with the needle tip within the pes anserine bursa, which lies in between the pes anserine tendons and superficial fibers of the MCL. Care should be taken to avoid injecting deep to the MCL as this would be intraarticular.

This is a transverse midfoot image of the metatarsal (MT) bases during an injection of the intermetatarsal joint between the fourth and fifth metatarsals (4-5 IM). The needle can be seen traversing dorsal lateral to plantar medial in-plane with the needle tip deep to the 4-5 dorsal MT ligament within the 4-5 IM joint. Ultrasound is very useful for precise localization in midfoot joint injections, making it valuable for both diagnostic and therapeutic purposes. For performing midfoot injections in-plane such as this one, a gel standoff is helpful for needle visualization.
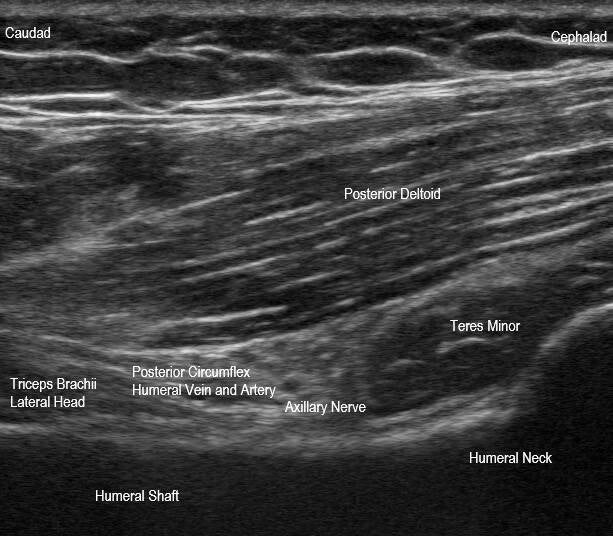
This is an anatomic sagittal plane image of the quadrilateral space, posterior to the teres major. The quadrilateral space contains the posterior circumflex humeral vasculature and axillary nerve. Its boundaries include the teres minor superiorly, teres major inferiorly, long head triceps brachii medially, and surgical neck of the humerus laterally. In rare circumstances, the neurovasculature can become compressed in quadrilateral space syndrome, which can result in posterolateral shoulder pain. In this image, interventions can be performed such as an axillary nerve block, which is typically performed in-plane in a cephalad posterior to caudad anterior approach.

This is an anatomic transversal plane view of the posterior glenohumeral joint during a glenohumeral joint injection. The needle can be seen traversing posterolaterally to anteromedially in-plane through the posterior deltoid and infraspinatus with the needle tip visualized within the posterior glenohumeral joint recess. This procedure is usually best performed using a curvilinear transducer to help best visualize the needle in a steep angle. It is usually best to angle the needle in a way to just bypass over the humeral head cartilage to target the posterior recess and avoid puncturing the posterior glenoid labrum.

This is a long axis image of the plantar fascia central cord at the medial calcaneal tubercle. There is an anechoic defect consistent with a high grade partial thickness undersurface tear of the plantar fascia. Additionally there is hypoechoic thickening and loss of normal fibrillar echotexture of the plantar fascia central cord at the origin consistent with fasciosis. Greater than 4 mm thickness (at medical calcaneal tubercle) suggests abnormal thickening. Orthogonal view in short axis should be evaluated to determine the width of the tear. Dynamic assessment with great toe extension can improve visualization of the proximal portion of the plantar fascia, by straightening due to the windlass mechanism. A tear at this location can be seen in chronic cases of plantar fasciosis due to degeneration. Keep in mind you will likely need to adjust the time gain compensation to improve visualization when evaluating the plantar fascia due to the attenuation from the thick plantar skin and heel pad.


Create Your Own Website With Webador